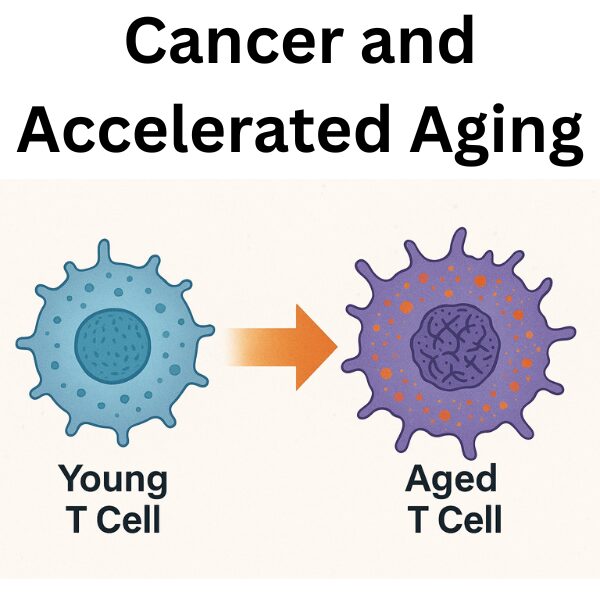
In recent years, cancer and aging have increasingly been understood not as separate biological phenomena, but as interconnected processes. Immune decline and chronic inflammation in cancer patients may not be caused solely by treatment side effects, but also by tumors themselves, which can drive aging-like phenotypes in host cells and tissues. In this article, we review the landmark study “Lymphoma accelerates T cell and tissue aging” (Hesterberg et al., Cancer Cell, 2025) from the John Cleveland laboratory, and place it in the context of the Hallmarks of Aging to provide a systematic overview of how cancer promotes molecular and cellular aging.
Defining Aging and the Hallmarks of Aging
Aging is not simply the passage of time, but rather a set of molecular and functional alterations within cells and tissues. The framework of the Hallmarks of Aging, proposed by López-Otín and colleagues, has become a cornerstone for conceptualizing age-related biology.
Major Hallmarks of Aging (2013 / 2023 update)
- Genomic instability
- Epigenetic alterations
- Loss of proteostasis
- Deregulated nutrient sensing (mTOR, IGF signaling)
- Mitochondrial dysfunction
- Cellular senescence
- Stem cell exhaustion
- Inflammaging (chronic low-grade inflammation)
- Recent additions: disrupted intercellular communication, circadian deregulation, metabolic homeostasis failure
The 2025 Cancer Cell study highlights four central features induced by cancer in young T cells: epigenetic alterations, proteostasis defects, inflammaging, and iron dysregulation.
Cancer and Aging: Established Perspectives
Traditionally, research on cancer and aging has focused on two main domains:
- Treatment-induced accelerated aging: Radiation, chemotherapy, and bone marrow transplantation cause DNA damage and epigenetic reprogramming, leading to premature aging in survivors (Ness et al., 2018).
- Cancer-driven systemic aging: Tumor-derived factors and metabolic competition can induce senescence-like states in host immune cells and tissues (Freund et al., 2010).
The John Cleveland Group Study (Cancer Cell, 2025)
Study Overview
Hesterberg and colleagues used mouse models of B cell lymphoma and T cells from human diffuse large B cell lymphoma (DLBCL) patients to test whether tumors themselves can drive immune aging. Their analysis combined flow cytometry, scRNA-seq, and ATAC-seq.
Key Findings
- Young T cells exposed to lymphoma rapidly adopted aging phenotypes, including increased CD39, PD-1, KLRG1, and FOXP3 expression.
- Epigenetic profiling revealed activation of heme metabolism and iron homeostasis pathways uniquely in young T cells.
- Lymphoma provoked iron accumulation (Fe²⁺) and ferroptosis resistance, driving functional aging.
- Young mice with lymphoma displayed increased Cdkn2a and Tnfa expression in kidneys and aorta, reflecting tissue-level senescence.
- Some aging phenotypes (e.g., cytokine overproduction) were reversible after tumor clearance, while others (iron dysregulation, proteostasis defects) were fixed.
Comparison with Related Studies
While many reports link cancer therapies to accelerated aging, this study is unique in showing that tumors alone can directly shift young immune cells toward aged phenotypes. This distinction is a major conceptual advance.
Implications for Future Research and Therapy
The findings carry broad translational implications:
- Immunotherapies (CAR-T, checkpoint inhibitors) may be limited by tumor-driven immune aging.
- Targeting ferroptosis, proteostasis, or epigenetic alterations may offer novel combined anti-cancer and anti-aging strategies.
- Survivorship care must recognize that some tumor-driven aging phenotypes are irreversible and require proactive management.
Author’s Perspective
From my perspective, this study reframes cancer as not only a proliferative disease but also as a driver of accelerated systemic aging. The convergence of iron metabolism and epigenetics is particularly promising as a therapeutic target. In the future, a dual-therapy model—combining anti-cancer and anti-aging interventions—may become a central strategy in oncology and geroscience.
References
- López-Otín C, et al. “The Hallmarks of Aging.” Cell, 2013.
- López-Otín C, Kroemer G. “Hallmarks of Health and Ageing.” Nat Rev Mol Cell Biol, 2023.
- Hesterberg RS, et al. “Lymphoma accelerates T cell and tissue aging.” Cancer Cell, 2025.
- Ness KK, et al. “Physiologic frailty as a sign of accelerated aging among adult survivors of childhood cancer.” J Clin Oncol, 2018.
- Freund A, et al. “Inflammatory networks during cellular senescence: causes and consequences.” Nat Rev Cancer, 2010.
- Masaldan S, et al. “Iron accumulation in senescent cells.” Nat Commun, 2018.
- Ghosh AK, et al. “Aging-associated iron dysregulation impairs T cell immunity.” Blood, 2021.
Related articles



This article was edited by the Morningglorysciences team.


Comments